Can Stress Cause Hemorrhoids?
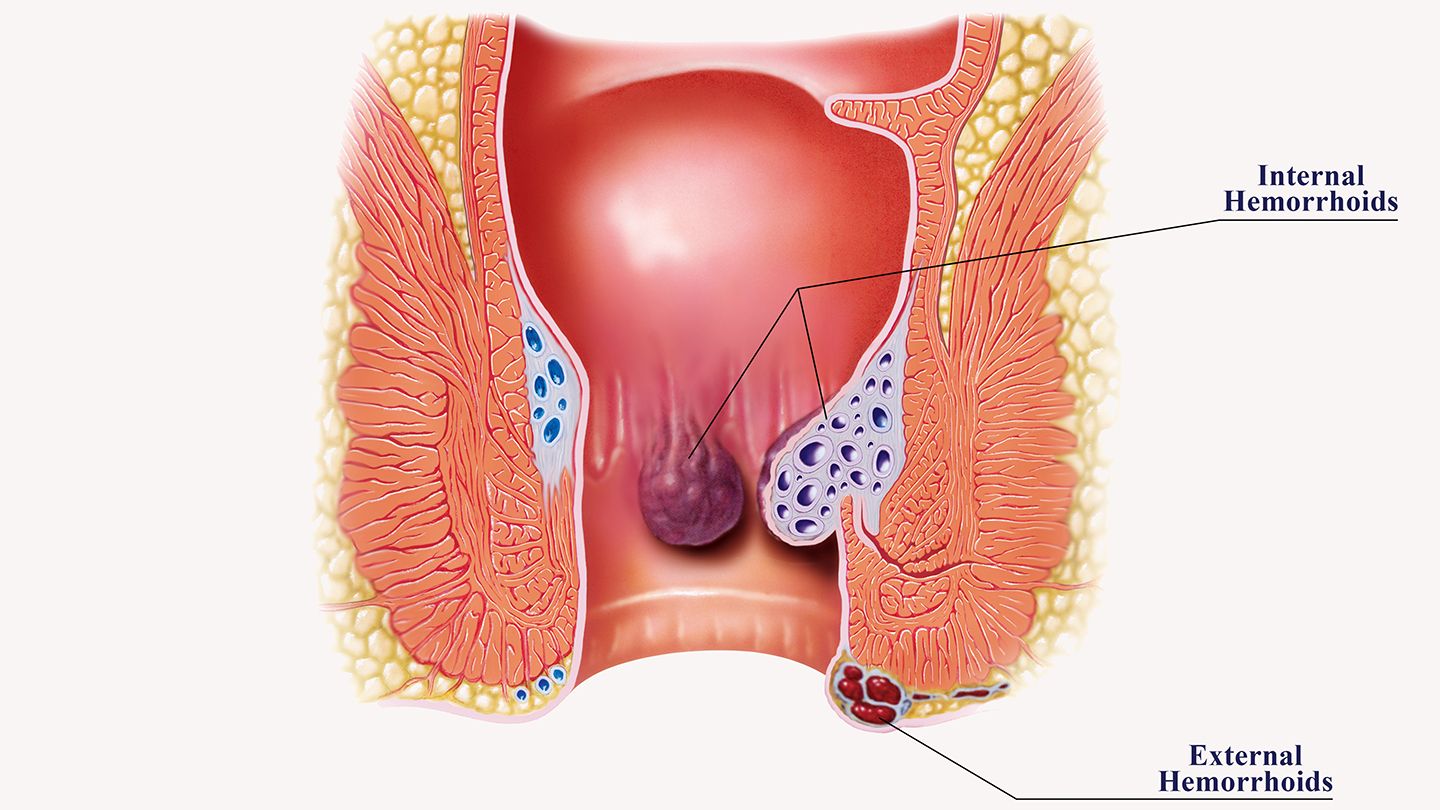
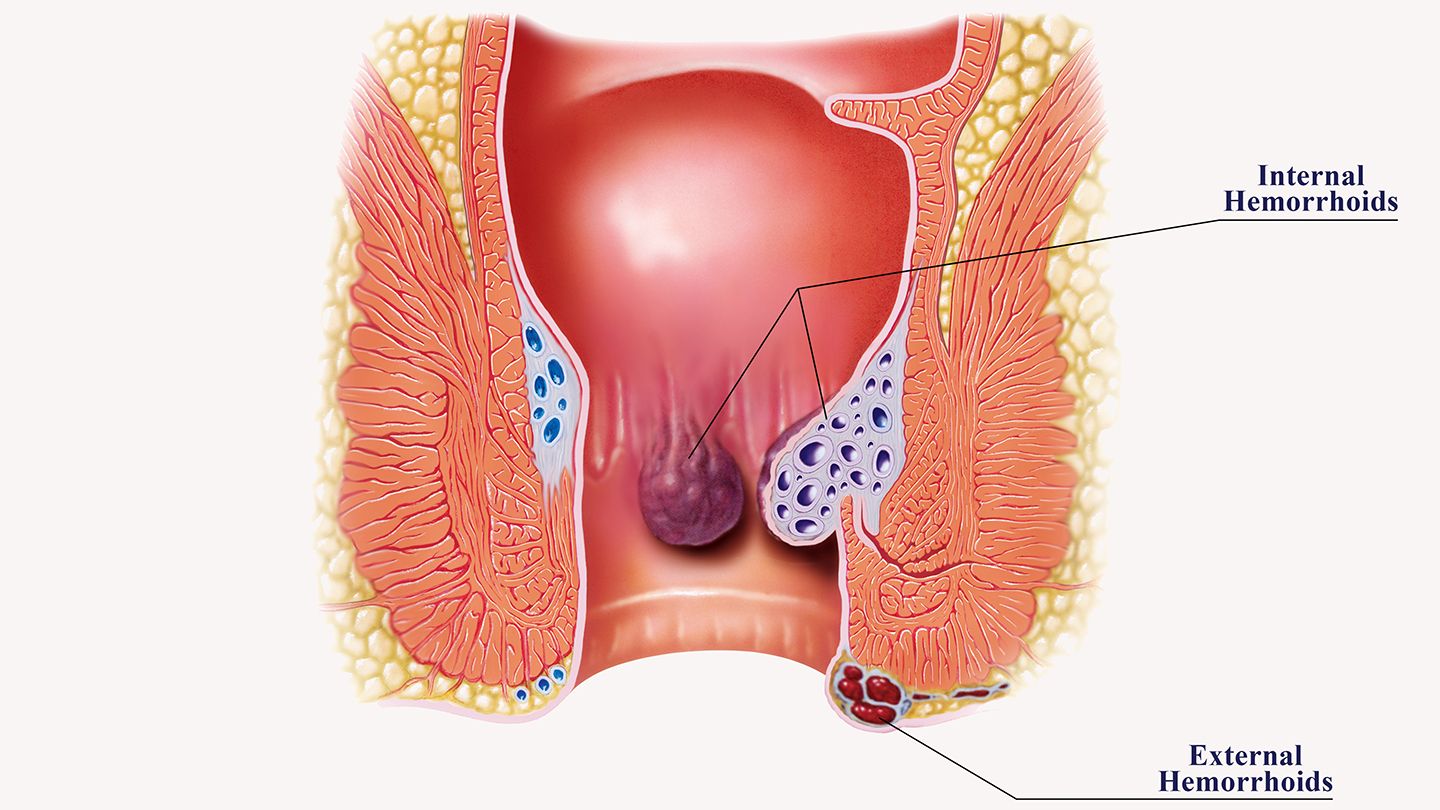
Hemorrhoids are enlarged veins located in the lower rectum or around the anus. They frequently cause symptoms like irritation, discomfort and bleeding. Some research suggests stress may increase hemorrhoid risk. But how exactly are stress and hemorrhoids connected?
Understanding Hemorrhoids
Hemorrhoids affect around 1 in 20 Americans. They most often develop from increased pressure in the lower rectum. Contributing factors include:
- Chronic constipation and straining
- Diarrhea
- Sitting for long periods
- Obesity
- Pregnancy
- Aging
Hemorrhoids are classified as internal or external depending on location. Internal hemorrhoids form in the rectum itself, while external hemorrhoids occur under the skin around the anus. Both types can cause problems like:
- Itching and irritation
- Swelling
- Pain or discomfort
- Bleeding, especially with bowel movements
- Leakage of stool or mucus
Hemorrhoid symptoms range from mild to severe based on size and whether a clot has formed. Home treatments can relieve many mild cases. More advanced hemorrhoids may require procedures or surgery.
How Might Stress Contribute to Hemorrhoids?
Research exploring the connections between stress and hemorrhoid development is limited. But some potential ways stress could increase risk include:
1. Gastrointestinal Changes
Stress significantly impacts gastrointestinal function. Under stress, processes like digestion, absorption and elimination can slow down or speed up. This may lead to constipation or diarrhea, both hemorrhoid risk factors.
2. Poor Diet Quality
People under chronic stress often eat more impulsively and make less healthy food choices. Diets low in fiber and high in processed foods exacerbate constipation and straining during bowel movements.
3. Dehydration
When stressed, people frequently forget to drink enough water. Dehydration from inadequate fluid intake can make constipation worse and harden stools, increasing hemorrhoid risk.
4. Blood Flow Changes
Stress hormones like cortisol and adrenaline affect circulation. Sustained stress could plausibly impact blood flow in the rectal veins, potentially contributing to hemorrhoid swelling and inflammation.
5. Increased Anal Sphincter Tension
Psychological stress may increase tension in the external anal sphincter muscle. Chronic tightening of this muscle could theoretically raise pressure on rectal veins and lead to hemorrhoids.
6. Weakened Immune Function
Stress suppresses immune defenses which could delay healing of existing hemorrhoids. Prolonged flare-ups may increase complications like clots, tissue death and infection.
7. Sedentary Lifestyle
People under chronic stress are less likely to exercise and move regularly. Lack of physical activity increases hemorrhoid risk factors like constipation and pressure on the perineum.
Overall, the exact mechanisms linking stress and hemorrhoids require more research. But there are plausible ways psychological stress could predispose someone to developing hemorrhoids through physical changes.
Research Connecting Stress and Hemorrhoids
Some studies provide evidence that psychological stress may increase hemorrhoid risk:
- A 2010 study found anxiety was significantly higher in people with hemorrhoids vs healthy controls.
- A 2015 study reported negative life events increased hemorrhoid risk while exercise lowered risk.
- A 2016 study showed anxiety, depression and sleep issues occurred more often in people with hemorrhoids.
- A 2019 study linked higher perceived stress scores with increased hemorrhoid symptoms.
Additionally, research shows anti-anxiety medications like diazepam help reduce anal sphincter hypertonia and painful spasms after hemorrhoid surgery. This indicates reducing stress may aid hemorrhoid healing.
Overall, while research is limited, some studies suggest higher stress levels correlate with greater incidence and severity of hemorrhoids.
Types of Stress That May Influence Hemorrhoids
Both acute and chronic stress could plausibly impact hemorrhoid development:
Acute Stress
Short-term stressors like public speaking, injuries or conflicts could transiently worsen constipation, diet and fluid intake. Frequent acute stress may increase cumulative hemorrhoid risk.
Chronic Stress
Ongoing sources of stress like work, relationships, finances or caregiving may chronically elevate cortisol, alter GI function, restrict activity and weaken immunity. This sustained stress likely has stronger hemorrhoid effects.
Perceived Stress
How a person perceives and reacts to stressors also matters. Those viewing events negatively with excessive worry may experience more physical effects from stress, including higher hemorrhoid risk.
Both external stressful events and your internal responses to stress should be well managed to minimize the chances of developing hemorrhoids.
Populations Vulnerable to Stress-Related Hemorrhoids
Certain populations seem especially vulnerable to hemorrhoids under high stress. Groups at increased risk include:
- Anxious individuals - Existing anxiety disorders may amplify stress responses.
- Depressed individuals - Depression often increases stress sensitivity.
- Women - Hormonal fluctuations related to menstruation, pregnancy and menopause appear to increase susceptibility.
- Adults over 50 - Aging-related connective tissue changes may worsen hemorrhoids under stress.
- People with IBS - Irritable bowel syndrome amplifies GI changes from stress that may provoke hemorrhoids.
Those already at higher hemorrhoid risk due to lifestyle factors like obesity and inactivity have increased vulnerability to added stress.
Tips to Prevent Stress-Related Hemorrhoids
Making smart lifestyle choices may help lower your chances of developing hemorrhoids under stress:
Exercise Regularly
Aim for 30+ minutes of activity like walking, swimming or yoga most days. Exercise improves gut motility, reduces pressure on rectal veins and manages stress.
Eat More Fiber
Focus on fruits, vegetables, whole grains, beans and nuts. Fiber softens stools and prevents straining that leads to hemorrhoids.
Stay Hydrated
Drink plenty of water and limit caffeine and alcohol to keep your GI system functioning optimally.
Take Probiotics
These healthy gut bacteria facilitate regular, easy bowel movements and lessen diarrhea and constipation from stress.
Try Biofeedback
This technique helps control physiological responses to stress through relaxation and mental focus. It may decrease anal sphincter pressure.
Practice Stress Management
Try yoga, mindfulness, calming hobbies and other stress relief strategies. Getting stress under control minimizes negative physical effects.
Use Squat Toilets
Elevating your feet simulates a squat position that straightens the anorectal angle and reduces straining.
Take Warm Baths
Sitting in warm water can relieve constricted anal sphincter muscles and decrease swelling.
Adopting preventive habits reduces the chances that stress will trigger or worsen bothersome hemorrhoids.
Medical Treatments for Hemorrhoids
Several medical interventions can treat painful or bleeding hemorrhoids:
Medications
Stool softeners, fiber supplements, vasoconstrictors and analgesic creams can relieve mild symptoms.
Minimally Invasive Procedures
Rubber band ligation, sclerotherapy injections and infrared coagulation can eliminate grade 1 and 2 hemorrhoids in the doctors office.
Surgery
Hemorrhoidectomy, Doppler guided ligation and stapled hemorrhoidopexy are options for severe grade 3 or 4 hemorrhoids.
Discuss all medical and procedural options thoroughly with your doctor to determine the best hemorrhoid treatment plan for your situation.
When to See a Doctor
Visit your healthcare provider for evaluation if you have:
- Bleeding not relieved by over-the-counter treatments
- Severe pain or swelling
- Prolapse (hemorrhoid falling out of anal canal)
- Thrombosis (blood clot)
- Changes in bowel habits
- Anemia from blood loss
Seeking prompt medical care is important if hemorrhoid symptoms are significantly impacting your daily life. Dont assume symptoms are just from stress without getting evaluated.
Stress Management Strategies for Hemorrhoids
Once you have hemorrhoids, effectively managing stress is essential to prevent flare-ups and promote healing. Helpful stress relief approaches include:
Relaxation Techniques
Try breathwork, visualization, progressive muscle relaxation, meditation and yoga to turn off the stress response.
Cognitive Restructuring
Identify and reframe negative thoughts contributing to worry and perceived stress.
Social Support
Spend time with encouraging friends and family to buffer stress effects.
Therapy
Counseling can provide valuable perspective on stress and teach coping strategies.
Lifestyle Changes
Adjusting exercise, diet, sleep and recreational habits can improve resilience.
Learning to actively manage stress helps you minimize aggravating hemorrhoid symptoms and prevent recurrences.
The Bottom Line
Research suggests high stress levels may increase the risk for developing hemorrhoids. Both acute and chronic stress can plausibly contribute through mechanisms like constipation, immunity changes, sedation and blood flow disruption.
However, limited studies exist on the exact relationship between psychological stress and hemorrhoid formation. More research is needed to confirm a direct cause and effect link.
Nonetheless, effectively managing stress and adopting a healthy lifestyle remain wise precautions to help you avoid hemorrhoids. Decreasing stress is also prudent after a hemorrhoid diagnosis to prevent aggravating symptoms during the healing process.
FAQs
How might stress lead to hemorrhoids?
Potential ways stress may increase hemorrhoid risk include worsening constipation or diarrhea, decreasing immunity, reducing blood flow, tightening anal sphincter muscles, and promoting inactivity and poor diet.
What types of stress affect hemorrhoids?
Both acute stress (short-term events) and chronic stress (ongoing difficulties) can impact factors like bowel habits, circulation, and immunity that may raise hemorrhoid risk.
Are certain people more vulnerable to stress-related hemorrhoids?
Those more prone to stress-induced hemorrhoids include anxious individuals, women, older adults, depressed people, those with IBS, and people who already have unhealthy lifestyles.
How can I prevent stress from causing hemorrhoids?
Tips to reduce stress-related hemorrhoid risk include regular exercise, eating more fiber, staying hydrated, taking probiotics, practicing relaxation techniques, and using squat toilets.
Should I see a doctor for possible stress hemorrhoids?
Yes, visit your doctor if you have persistent hemorrhoid symptoms like pain, swelling, bleeding, or changes in bowel habits. Don’t assume symptoms are just from stress without being evaluated.
Disclaimer: This article is for informational purposes only and does not constitute medical advice. Always consult with a healthcare professional before starting any new treatment regimen.
Related Coverage
Obesity can make wiping after a bowel movement difficult. Adjusting technique, using tools, and requesting assistance when needed allows proper hygiene....
Many pregnant women safely bowl with proper precautions like using lighter balls, appropriate shoes, hydrating, and avoiding smoke-filled alleys. Learn expert advice on bowling while pregnant....
If you spot something resembling a kidney bean in the toilet after a bowel movement, it likely signals protruding hemorrhoids. Learn what causes them and treatment options....
Research suggests high stress levels may increase hemorrhoid risk. Stress can contribute through mechanisms like constipation, immunity changes, and blood flow disruption....
Abortions often cause constipation after from hormones, dehydration and medications. Tips to relieve and prevent painful post-abortion constipation at home safely....
Learn whether hemorrhoids can lead to prostate pain and urinary issues. Understand the indirect links between hemorrhoid swelling and prostate inflammation....
Learn about hemorrhoid symptoms, causes, home treatments, and when to consider hemorrhoid banding at home. Get step-by-step instructions on how to use a home hemorrhoid banding kit....
Hemorrhoids are swollen veins in the anus that can cause bleeding and pain. Learn about hemorrhoid causes, treatments, surgery, and prevention tips for men....
Wondering what hemorrhoid surgery recovery is like day-by-day? See photos and get the facts on pain, activity, bowel movements, and more for each stage of healing after hemorrhoid procedures....
Don't let others limit you with labels, stereotypes and comparisons. Heal past pain, build confidence, follow passions - you are meant for greatness....