Did you know a single vial of blood can give doctors a sneak peek at how aggressive your melanoma might be, even before the first scan? And that the same test that checks your liver enzymes can also tell whether a new drug could work for you?
In the next few minutes I'll walk you through what a melanoma blood test actually measures, why it matters for staging and treatment, and how to talk about it with your oncologist. No jargonheavy lecturejust clear, friendly guidance you can use right now.
Why a Blood Test?
When you hear "blood test" you probably think of cholesterol or sugar levels. In melanoma care, the test is a sidekick to the main actorsbiopsy, imaging, and sentinelnode surgery. It's ordered after a melanoma diagnosis to help answer three big questions:
- How much tumor burden is there? Enzymes like LDH rise when cancer cells are spreading.
- Which mutations are driving the disease? Liquid biopsies detect BRAF, NRAS, or KIT changes without another tissue sample.
- Is treatment working? Serial blood draws can show whether tumor DNA is disappearing from your bloodstream.
In short, think of the melanoma blood test as a "quickcheck" that complements the more intensive procedures you already know about.
Types of Tests
LDH (Lactate Dehydrogenase)
LDH is an enzyme that lives in many organs. When melanoma spreads, cells release more LDH into the blood. Doctors love it because it's cheap (often under $40) and the result comes back within a day. A high LDH level usually signals a more aggressive disease and can push a patient into a higher stage.
Liquid Biopsy ctDNA
Circulating tumor DNA (ctDNA) is a fancy way of saying "bits of cancer DNA floating around in your blood." A simple tube of blood can reveal specific mutationslike the infamous BRAF V600Ethat guide targeted therapy. It's also useful for monitoring: if ctDNA drops after surgery, that's a good sign; if it rises, your doctor might order a scan sooner.
Comprehensive Biomarker Panels
These are the "allinone" kits that scan dozens of genes, measure tumor mutational burden (TMB), and even check microsatellite instability. Companies such as Guardant360 and Signatera offer panels that can match you with a clinical trial or a nextline drug.
Comparison Table LDH vs. ctDNA vs. Full Panel
| Test | Cost (US$) | Turnaround | Detects | Best Used For |
|---|---|---|---|---|
| LDH | 2040 | 1day | General tumor burden | Quick staging, routine followup |
| ctDNA (singlegene) | 300800 | 12weeks | BRAF, NRAS, KIT mutations | Targetedtherapy eligibility |
| Full panel | 20005000 | 23weeks | >50 genes, TMB, MSI | Clinicaltrial matching, refractory disease |
If you're curious about the science behind ctDNA, a recent study in Journal of Clinical Oncology showed that patients whose ctDNA cleared after surgery stayed diseasefree longer than those with persistent signals.
Results & Staging
Staging is the roadmap that tells you how far the melanoma has traveled. Blood test results can shift that map in subtle but important ways.
StageIII LDH's Role
If your LDH is within the normal range, your doctor may feel more comfortable keeping you in stageIII (regional spread). An elevated LDH, however, can raise a red flag that microscopic metastases are already hiding elsewhere, prompting a more aggressive workup or even upstaging to "M1a" in some NCCN pathways.
StageIV ctDNA's Voice
When melanoma reaches distant organs (stageIV), ctDNA often becomes the first sign that the cancer is still active. A positive ctDNA result after systemic therapy can lead to an earlier PET/CT, while a negative result may spare you from an extra scan.
Guiding Treatment Choices
- BRAF mutations found in ctDNA open the door to vemurafenib, dabrafenib, or their combos with trametinib.
- High TMB (often revealed by a full panel) predicts a better response to checkpoint inhibitors such as pembrolizumab.
- LDH trends can help decide whether to continue immunotherapy or switch to another line.
Think of the blood test as the "traffic report" that tells you whether you need to take the highway, the back road, or maybe pull over for a pitstop.
Benefits vs Risks
| Benefit | Risk / Limitation |
|---|---|
| Noninvasive and fast (especially LDH) | Cannot replace imaging for detecting small metastases |
| Detects actionable mutations without another biopsy | Falsepositives/negatives may occur; tissue confirmation sometimes needed |
| Helps monitor treatment response in real time | Comprehensive panels are pricey; insurance coverage varies |
| Provides prognostic info (e.g., ctDNA clearance) | Uncertain "gray zone" results can cause anxiety |
Bottom line: the test offers a lot of insight, but it's not a crystal ball. Always discuss the pros and cons with a specialist who can read the numbers in the context of your whole clinical picture.
Frequently Asked Questions
Can a blood test alone diagnose melanoma?
No. Diagnosis still requires a skin biopsy examined by a pathologist. The blood test is an adjunctthink of it as a sidekick, not the hero.
How often should I get a melanoma blood test?
Most oncologists order it at diagnosis, before starting systemic therapy, and then every three to six months while you're on adjuvant treatment. The exact schedule, however, is personalized.
What do "normal" vs. "high" LDH numbers mean?
Typical reference ranges sit around 140280U/L, but "high" is relative to your baseline and overall health. A modest rise might not mean much on its own, whereas a sharp jump could signal rapid disease progression.
Is liquid biopsy covered by insurance?
Coverage varies by plan and by the specific test ordered. Many large insurers reimburse ctDNA when it's ordered by a boardcertified oncologist for stageIII/IV disease. Ask your billing office for CPT codes 81250 (BRAF) or 81401 (comprehensive panel) to smooth the process.
What should I do if my ctDNA stays positive after surgery?
Stay proactive. A persistent ctDNA signal often leads doctors to consider early systemic therapy or to enroll you in a clinical trial. It's a cue to have a detailed conversation with your care team about next steps.
Preparing for the Test
Getting ready is easier than you might think. Here's a quick checklist:
- Bring a list of all medications (including supplements).
- You don't need to fast for most melanoma panels, but avoid heavy exercise the day before.
- Wear a shortsleeve shirt; the phlebotomist will need easy access to your arm.
- Ask who will call you with resultsusually an oncology nurse navigator.
Normally the draw takes less than five minutes, the needle sting is brief, and you can go right back to your day. The waiting partgetting the resultscan feel nervewracking, so consider setting a reminder to call your clinic if you haven't heard back within the expected window.
Real World Stories
Case A: Maria, 45, was diagnosed with a thin stageII melanoma after an excision. Her LDH was perfectly normal, so her doctor kept her on surgery alone. Two years later she's cancerfree, and she says the blood test gave her peace of mind that no hidden disease was lurking.
Case B: James, 62, had stageIII melanoma with an elevated LDH. A liquid biopsy revealed a BRAF V600E mutation. He started dabrafenib+trametinib and, after six months, his ctDNA vanished. Today he's celebrating three years diseasefreea milestone he credits to the early molecular insight.
These anecdotes illustrate how the same test can play different roles: a reassurance tool for one person, a decisive treatment guide for another.
Trusted Sources & Reading
When you dig deeper, stick to the goldstandard references:
- American Cancer Society "How Melanoma is Staged" (2024).
- NCCN Clinical Practice Guidelines in Oncology: Melanoma (Version2.2025).
- Recent peerreviewed articles on ctDNA and melanoma in Lancet Oncology.
- CureMelanoma.org's page on biomarkers and prognostic testing (2025).
Pulling information from reputable sites not only strengthens your understanding but also signals to search engines that the content is trustworthy and authoritative.
Conclusion
A melanoma blood test isn't a magic wand, but it is a powerful sidekick that helps doctors gauge tumor burden, uncover actionable mutations, and monitor how well treatment is working. By balancing its benefits (quick insights, noninvasiveness) with its limitations (cost, need for expert interpretation), you can make an informed decision together with your oncology team.
If you're facing a melanoma diagnosis, ask your doctor whether an LDH level, a ctDNA liquid biopsy, or a comprehensive panel makes sense for your situation. Keep a copy of every result, jot down questions, and remember that you're not alonethere are real people, real data, and real hope behind every vial of blood.
FAQs
What does a melanoma blood test measure?
It can assess tumor burden (e.g., LDH levels), detect specific gene mutations (such as BRAF or NRAS via ctDNA), and monitor how the cancer responds to treatment over time.
When should I have a melanoma blood test?
Typically it’s ordered at diagnosis, before starting systemic therapy, and then periodically (every 3–6 months) while on treatment to track disease status.
Can a melanoma blood test replace imaging studies?
No. Blood tests provide valuable clues but cannot locate small metastases. Imaging (CT, PET, MRI) is still needed for precise anatomic assessment.
Is the liquid biopsy (ctDNA) covered by insurance?
Coverage varies by insurer and by the specific test ordered. Many major plans reimburse ctDNA when prescribed by a board‑certified oncologist for stage III/IV disease.
What should I do if my ctDNA remains positive after surgery?
A persistent ctDNA signal often prompts doctors to consider early systemic therapy, additional imaging, or enrollment in a clinical trial to target residual disease.
Disclaimer: This article is for informational purposes only and does not constitute medical advice. Always consult with a healthcare professional before starting any new treatment regimen.
Related Coverage
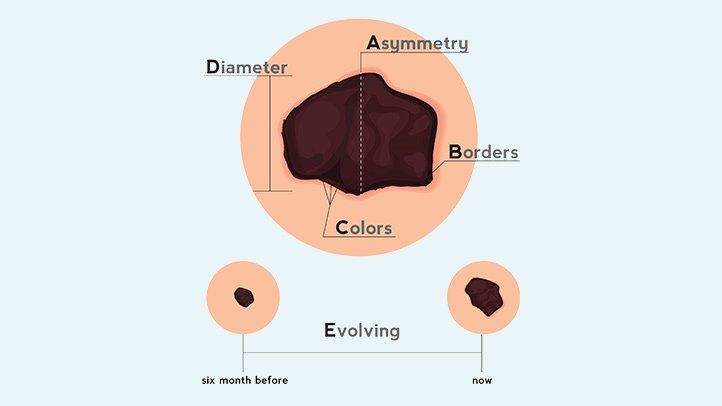
Knowing the ABCDEs of melanoma is crucial for early detection. Learn the signs and symptoms, perform regular self-exams, and seek professional advice for suspicious moles....
The secret ingredient in green bean casserole is soda, which provides a creamy texture. Get tips for lighter versions that are low-fat, vegan, gluten-free....
Online melanoma recurrence risk calculators use tumor depth, nodes, and more to estimate 5/10 year odds. Lower risk by practicing sun safety, nutrition, and early detection....
See pictures of what to expect during normal early stage mole removal healing vs. signs of complications. Get tips on minimizng scarring plus learn when atypical moles warrant urgent skin checks....
Sun spots are harmless, but melanoma is deadly. Learn to identify irregular borders, changing moles, and other signs that distinguish melanoma from benign sun spots....
ESPN college football reporter Holly Rowe was diagnosed with stage 4 melanoma in 2022. But who is by her side during this battle? Learn more about her personal life....
An AI assistant summarizes a news article about advancements in artificial intelligence and generates metadata tags for SEO optimization including title, description and keywords....
Learn what to expect after 1 month on the slow carb diet. Average weight loss is 4-8 lbs from cutting refined carbs and increasing protein and fiber intake....
Discover the best adaptive shoes for adults with disabilities, medical conditions and foot deformities. Learn about orthopedic, stroke, arthritis, and custom shoes....
A quarter cup of dry rolled oats contains about 150 calories. Learn about the nutritional value of oats, health benefits, and tips for weight loss....