At first, I thought it was nothingjust a little blood on the toilet paper. Maybe you've had that moment too: a flash of worry, a dozen questions, and a quick Google search. Internal hemorrhoids symptoms can be subtle, and knowing what's normal versus what deserves a check-up truly matters.
Here's the quick take: internal hemorrhoids most often cause painless rectal bleeding, itching, and sometimes a prolapsed hemorrhoid. Most flares calm down with smart self-care at home. Some need a doctor's help. In this guide, we'll break down what to look for, when to worry, and the safest treatmentstold plainly, with warmth, and without the scare tactics.
What symptoms mean
Let's start simple: internal hemorrhoids are swollen veins inside the rectum. Because they're higher up, they usually don't have pain fibers like the skin around the anus does. That's why the most common signal is blood you seebut don't feel.
Most common signs
Painless bleeding is the classic calling card. You might notice bright red streaks on toilet paper, in the toilet bowl, or coating the stool. Some people describe a sense of fullness or pressure, as if there's something there after a bowel movement. Hemorrhoid itching is also commonespecially if mucus makes the skin moist and irritated.
What "painless rectal bleeding" usually looks like
Picture this: you wipe, and there's bright red blood. Or you glance into the bowl and see pinkish water. It's usually smaller amountsthink smears or a few drops. It tends to show up with bowel movements and settles when the flare improves. That said, any rectal bleeding deserves attention if it lasts more than a couple of weeks, is heavy, or is new for you.
Hemorrhoid itching vs. skin irritation: how to tell
Itching from internal hemorrhoids often comes with moisture or mucus. Skin irritation, on the other hand, might be triggered by scented wipes, soaps, or aggressive cleaning. If it eases with gentle cleansing, drying, and a barrier cream (like zinc oxide or petroleum jelly), it may have more to do with skin than the hemorrhoid itself. If you're stuck in a scratch-itch cycle, it's a sign to simplify products and focus on moisture control.
Less common but important signs
Not everyone gets these, but they're worth knowing.
Mucus discharge, soiling, and moisture
Internal hemorrhoids can produce a little mucus. That can lead to dampness, mild soiling, and itching. It's annoying, yes, but usually manageable with gentle hygiene and breathable underwear.
Feeling of pressure or incomplete evacuation
Some people feel like they didn't "finish" after a bowel movement. That pressure can be a sign of engorged internal hemorrhoids or mild prolapse. If you notice this routinely, especially with constipation, consider it your gut asking for more fiber and fluids.
Pain: when internal hemorrhoids actually hurt
Internal hemorrhoids usually don't hurtbut there are exceptions. If a hemorrhoid prolapses (slips down) and gets swollen or trapped, it can be painful. A blood clot (thrombosis) in an external hemorrhoid hurts a lot, very suddenly. Anal fissures (tiny skin tears) can coexist and cause sharp, burning pain with bowel movements. If pain is new, severe, or persistent, check in with a clinician.
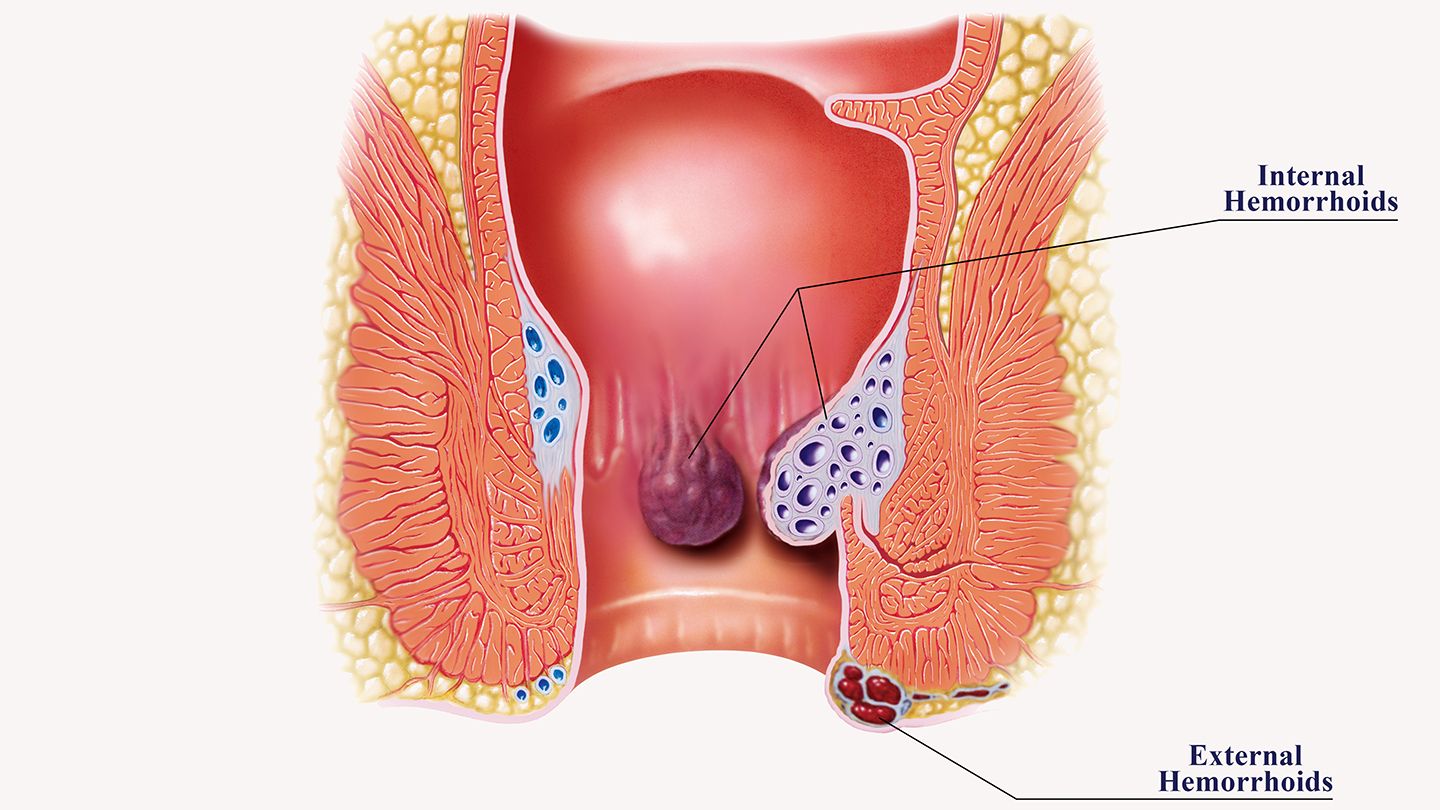
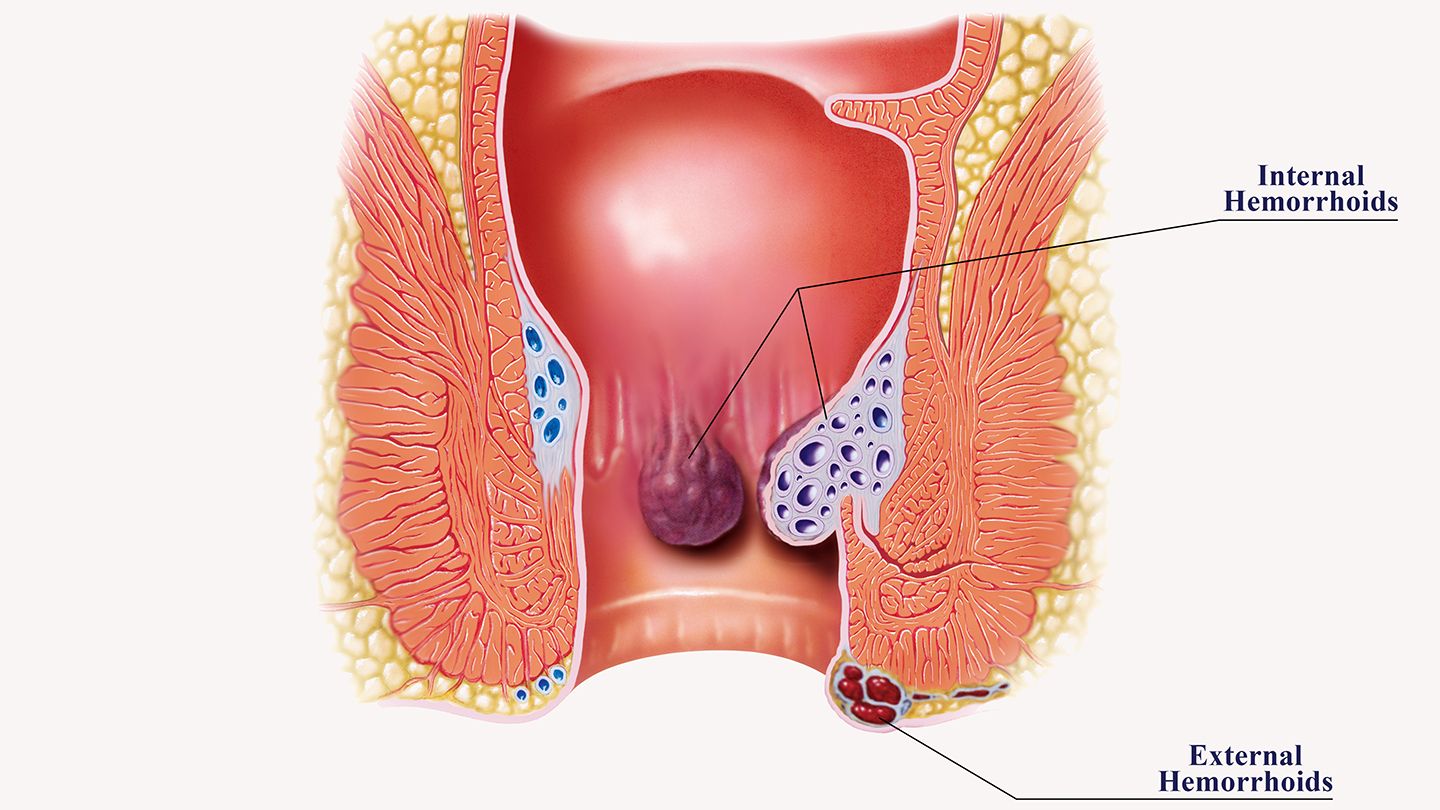
Internal vs external
Think of internal hemorrhoids as "inside the tunnel," and external ones as "on the edge of the tunnel." The location explains most differences.
Location and symptoms
Internal hemorrhoids: higher up, usually painless, bleeding is common, prolapse possible. External hemorrhoids: near the anal opening, you can feel the swelling, and pain is more likelyespecially if a clot forms.
Quick comparison list users can skim
Internal: painless bleeding, fullness/pressure, possible prolapse, mucus/itching from moisture. External: tender lump you can feel, sudden severe pain with clots, itching from skin irritation, less likely to bleed heavily unless irritated.
Why internal hemorrhoids can prolapse
Internal hemorrhoids are supported by connective tissue. Over timethanks to straining, constipation, pregnancy, or just gravitythat support can loosen. When you bear down, the hemorrhoid can slip lower (prolapse). Sometimes it slides back in on its own; sometimes it needs a gentle push; and sometimes it stays out.
Grading of prolapse (IIV) and what each feels like
Grade I: Stays inside; may bleed. Grade II: Prolapses with straining but goes back in by itself. Grade III: Prolapses and needs manual reduction (you gently push it back). Grade IV: Stays out and can't be reduced easilythis needs medical care.
Bleeding or something else
Here's the honest truth: hemorrhoids are common, but they're not the only cause of rectal bleeding. Age, family history, and new changes matter.
Red flags to act on
Seek care promptly for black or tarry stools, maroon blood mixed through the stool, dizziness or fainting, heavy bleeding with clots, or signs of anemia (fatigue, shortness of breath, pale skin). These are not typical internal hemorrhoids symptoms.
Conditions that mimic symptoms
Anal fissures cause sharp pain and bright red blood on toilet paper. Polyps and colorectal cancer can cause bleeding and changes in bowel habits. Inflammatory bowel disease brings inflammation, diarrhea, and bleeding. If you're over 45, have a family history of colorectal cancer, or notice unexplained weight loss or changes in stool caliber, it's time to talk with a clinician.
When age, family history, or new changes raise concern
New bleeding after age 45, or younger with significant family history, deserves evaluation. Persistent change in bowel habits, anemia, or unintentional weight loss should also prompt a closer look.
How clinicians checksafely and discreetly
Exams are usually quick and respectful: a visual inspection, a digital rectal exam, and often an anoscopy (a small lighted tube to see internal hemorrhoids). If bleeding is unexplainedor based on age and riskyour clinician may recommend a colonoscopy to rule out other causes. According to guidance from professional societies such as the American College of Gastroenterology and the American Society of Colon and Rectal Surgeons (see this patient overview from a colorectal surgery society), evaluation strategies balance symptoms, risk factors, and your comfort.
Treatment that works
I like to think of treatment in two phases: calm the current flare, then lower the odds of the next one. Small, consistent changes beat heroic, short-lived efforts.
Immediate self-care
Start with the basics. They're simple, safe, and surprisingly powerful.
Fiber goals and fluids
Aim for 2035 grams of fiber per day and at least 68 cups of non-alcoholic fluids. Fiber softens and bulks stool, reducing strain and irritation. Psyllium (a soluble fiber supplement) has some of the best evidence for easing constipation and hemorrhoid symptoms. Increase gradually over a week to avoid gas and bloating. If stools are still firm, a stool softener (like docusate) or an osmotic laxative (like polyethylene glycol) can help.
Sitz baths: how and how often
Sitz baths are wonderfully soothing. Use warm water (not hot) for 1015 minutes, 23 times daily and after bowel movements during a flare. No fancy additives neededjust water. The warmth relaxes the area, reduces spasm, and eases itching.
Topicals: what helps and what to limit
For itching and mild swelling, witch hazel pads can feel calming. Short courses of low-strength hydrocortisone (for example, 1%) can help with inflammation, but limit to 57 days at a time to avoid thinning the skin. If symptoms persist, talk to your clinician about prescription options tailored to internal hemorrhoids.
Office procedures if symptoms persist
When self-care isn't enoughespecially with recurrent bleeding or a prolapsed hemorrhoidoffice-based treatments are effective and quick.
Rubber band ligation (RBL)
RBL is the workhorse. A small band is placed at the base of the internal hemorrhoid to cut off blood flow. The tissue shrivels and falls off within a week, usually with minimal downtime. You might feel pressure or a dull ache for a day or two. Success rates are high for Grade IIII hemorrhoids, and repeat sessions are sometimes needed. Risks are uncommon but include bleeding, pain, and very rarely infection.
Sclerotherapy and infrared coagulation
Sclerotherapy involves injecting a solution to shrink the hemorrhoid. Infrared coagulation uses heat to scar the tissue and reduce blood flow. Both are good options for smaller internal hemorrhoids or for those who can't undergo banding. They tend to have slightly lower long-term effectiveness compared with RBL, but recovery can be even easier for some people.
Surgery when it's worth it
For large, persistent, or Grade IV prolapsed hemorrhoidsor when other options failsurgical approaches come into play. Hemorrhoidectomy removes the tissue; it's very effective but can be more painful during recovery. Stapled hemorrhoidopexy lifts and secures prolapsing internal hemorrhoids with typically less postoperative pain but a different risk profile. Decisions here are personal: symptom severity, downtime, cost, and your risk tolerance all matter. Your surgeon will walk through pros and cons with you.
Pain and bleeding control
For discomfort, acetaminophen is a safe first choice for many. NSAIDs (like ibuprofen) can help with pain but may increase bleeding risk for some. If you take aspirin or anticoagulants, never stop them without explicit guidance from your prescribing clinicianyour cardiovascular risk comes first. For bleeding that lingers, procedures like RBL can reduce episodes significantly.
Everyday prevention
The secret sauce is consistency. A few gentle habits go a long way.
Bathroom habits
Don't strain. Respond to the urgedon't delay. Keep toilet time short (ideally under 5 minutes)scrolling sessions can wait. A footstool can help straighten the anorectal angle, making bowel movements smoother. Afterward, pat dry with unscented paper or rinse gently, then pat. Consider a bidet or a squeeze bottle for sensitive days.
Wiping tips that protect skin
Avoid scented wipes and soaps. If you use wipes, choose unscented and alcohol-free. Finish by keeping the area drymoisture is the arch-nemesis of comfort down there.
Diet and lifestyle
Build your day around fiber: oats or chia in the morning, beans or lentils at lunch, vegetables and whole grains at dinner, and fruit for snacks. Soluble fiber (oats, psyllium, apples, beans) is especially soothing. Walk dailymovement nudges the gut awake. A simple routine like "coffee, short walk, bathroom" trains the bowels over time.
Movement and weight
Even 2030 minutes of walking helps keep stools moving and reduces pressure from prolonged sitting. If you sit at work, stand and stretch every hour. Small shifts, repeated daily, protect you far better than occasional overhauls.
Itching control without making it worse
Manage moisture with breathable cotton underwear and avoid tight, synthetic fabrics. Use a thin layer of barrier cream if the skin feels raw. If itching persists, step back from multiple productsthe simpler the routine, the calmer the skin.
Prolapse: what to do
So, what does a prolapsed hemorrhoid feel like? Often like a soft bump or bulge that appears during bowel movements. It may go back in on its own or need gentle help.
Signs you'll notice
A bulge with straining, mucus, irritation, and sometimes mild bleeding. The skin can get chafed if the tissue stays out. If it's tender and doesn't reduce, that's your cue to call a clinician.
Safe self-care vs help
For Grades IIIII, you can sometimes reduce the prolapse gently: wash your hands, use a dab of water-based lubricant, lie on your side, and softly press the tissue back through the opening. A cold compress can reduce swelling first. Don't force itif it won't go, stop. Severe pain, constant bleeding, or a prolapse that turns dusky or very swollen needs urgent care due to the risk of strangulation.
How doctors decide
Good care is a conversation. Your clinician will ask about your symptom timeline, bowel habits, any medications (especially blood thinners), family history, and what you've tried so far. They'll then tailor a plan: often conservative care first, with a low threshold to use office procedures if bleeding recurs or a prolapsed hemorrhoid keeps bothering you.
Shared decisions that fit your life
If you've had multiple flares or frequent bleeding, earlier banding might be reasonable. If downtime is hard for you, minimally invasive options may be best. Be sure to ask about cost, expected number of sessions, recurrence rates, and what recovery feels like day-by-day. Clear expectations make the whole process less stressful.
Risks and limits
Let's keep it balanced. Everything we do has trade-offsand you deserve to know them.
Potential downsides
Topical steroids can thin skin if used too long. Banding can cause a day or two of pressure or aching, and rarely bleeding or infection. Sclerotherapy and infrared coagulation may need repeat treatments. Surgery is highly effective but comes with more recovery discomfort and typical surgical risks. No option is perfect, but the right one for you will match your symptoms and goals.
When it's more than hemorrhoids
If bleeding persists beyond 23 weeks despite good self-care, if you become anemic, lose weight without trying, or notice narrowing of stools, push for evaluation. You can also ask directly for anoscopy or, based on age/risk, colonoscopyespecially if you're over 45 or have a family history.
How to advocate for yourself
Bring a short symptom diary: when bleeding happens, stool consistency (the Bristol stool chart helps), what you ate, and any straining. List your medications and supplements. Write down your top three questions. You're not being "difficult"you're being thorough, and that leads to better care.
Checklists and guides
Sometimes the hardest part is knowing where to start. Here's a simple, gentle plan you can follow this week.
1-minute symptom check
Likely hemorrhoids: bright red blood on paper or in bowl, little to no pain, itching with moisture, sense of fullness, symptoms tied to constipation or straining. Needs evaluation now: heavy bleeding, black stools, dizziness, severe pain, fever, anemia symptoms, age over 45 with new bleeding, family history of colorectal cancer.
7-day gentle plan to calm a flare
Day 12: Start psyllium (1 teaspoon once daily, then increase as tolerated). Drink a full glass of water with it. Take a warm sitz bath 23 times daily. Use witch hazel pads after bowel movements. If itchy or inflamed, use hydrocortisone 1% thinly twice daily for up to 57 days. Keep toilet time under 5 minutes; use a footstool.
Day 34: Add one more serving of soluble fiber (oats, beans, chia). Walk 20 minutes daily. If stools are still hard, consider an osmotic laxative. Keep sitz baths going. Avoid scented wipes; pat dry and use a barrier ointment if the skin feels raw.
Day 57: Reassess. If bleeding is easing and comfort is better, stick with the routine. If bleeding persists or a prolapsed hemorrhoid keeps slipping out, call your clinician to discuss office procedures like rubber band ligation.
What to prepare for a visit
Your questions (What's my grade? Is RBL right for me? How many sessions? Recovery time?), your meds list (especially anticoagulants), your symptom diary, and any family history. Knowing these details speeds up care and makes the appointment more productive.
A quick story
One reader told me, "Week one, I panicked every time I saw blood. Week two, I actually followed the planfiber, water, sitz bathsand the bleeding dropped off. By week three, I felt like myself again." That ebb and flow is normal. Progress isn't always a straight line, but it tends to show up when we're consistent with the basics.
Closing thoughts
Internal hemorrhoids symptoms often look like painless, bright-red bleeding, occasional itching, and sometimes a prolapsed hemorrhoidbut pain, heavy bleeding, or ongoing changes deserve a check. Most flares improve with fiber, fluids, sitz baths, and better bathroom habits. If that's not enough, office procedures like rubber band ligation can be quick, effective ways to stop recurrent hemorrhoid bleeding and reduce prolapse. Keep it balanced: these treatments help, but they aren't perfect, and it's okay to ask about options, risks, and what fits your life. If bleeding persists, worsens, or you're over 45 (or have risk factors), talk to a clinician about evaluation. What do you thinkdid this answer your biggest questions? Share your experiences, and if anything's still fuzzy, ask away. We're in this together.
FAQs
What are the most common internal hemorrhoids symptoms?
The hallmark sign is painless, bright‑red bleeding on toilet paper or in the bowl, often accompanied by itching, a feeling of fullness, or occasional mucus.
When should painless rectal bleeding be evaluated by a doctor?
Seek care if bleeding is heavy, lasts more than a few weeks, is accompanied by dizziness, anemia signs, black/tainty stool, or if you’re over 45 with new bleeding.
Can internal hemorrhoids cause pain?
Usually they don’t, but pain can appear if a hemorrhoid prolapses and becomes trapped, if it thromboses, or if another condition like an anal fissure is present.
What at‑home measures help relieve a flare?
Increase fiber (20‑35 g/day) and fluids, take warm sitz baths 2‑3 times daily, use witch‑hazel or a low‑strength hydrocortisone cream, and avoid straining on the toilet.
What office procedures are available for persistent internal hemorrhoids?
Rubber‑band ligation is the first‑line option, followed by sclerotherapy or infrared coagulation for smaller lesions; surgery is reserved for large or Grade IV prolapses.
Disclaimer: This article is for informational purposes only and does not constitute medical advice. Always consult with a healthcare professional before starting any new treatment regimen.
Related Coverage
If you spot something resembling a kidney bean in the toilet after a bowel movement, it likely signals protruding hemorrhoids. Learn what causes them and treatment options....
Many pregnant women safely bowl with proper precautions like using lighter balls, appropriate shoes, hydrating, and avoiding smoke-filled alleys. Learn expert advice on bowling while pregnant....
Frequent bowel movements and pooping a lot is common at 35 weeks pregnant due to physical and hormonal changes. Hemorrhoids are also likely as your uterus expands....
Obesity can make wiping after a bowel movement difficult. Adjusting technique, using tools, and requesting assistance when needed allows proper hygiene....
Learn the top anal bump causes, from hemorrhoids to warts, and know when to seek medical help. Tips for relief and prevention....
Abortions often cause constipation after from hormones, dehydration and medications. Tips to relieve and prevent painful post-abortion constipation at home safely....
Learn whether hemorrhoids can lead to prostate pain and urinary issues. Understand the indirect links between hemorrhoid swelling and prostate inflammation....
Research suggests high stress levels may increase hemorrhoid risk. Stress can contribute through mechanisms like constipation, immunity changes, and blood flow disruption....
Kidney stones and hemorrhoids share several common causes like dehydration and straining. Learn how passing kidney stones can also lead to hemorrhoids....
It's common to poop frequently in late pregnancy due to pressure, hormones, diet changes and anxiety. Learn what causes loose stool and how to find relief....