Quick Answer
Ankylosing spondylitis (AS) moves through three distinct phases early, progressive (midstage), and late each with its own pattern of pain, stiffness, and possible complications. Spotting the stage early lets you choose the right mix of medication, movement, and lifestyle tweaks before the spine starts to fuse.
What symptoms define early ankylosing spondylitis?
Early AS usually shows up as dull, aching pain in the lower back or hips that's worse after sitting and eases with gentle movement. Morning stiffness lasting 3060 minutes and tenderness over the sacroiliac joints are classic clues.
How does progressive ankylosing spondylitis differ from the early stage?
In the progressive stage the pain climbs higher up the spine, often reaching the shoulders, ribs, and heels, and you may notice fatigue, occasional fever, or eye inflammation (uveitis).
When does ankylosing spondylitis become "late stage"?
Latestage AS is marked by visible vertebral fusion (ankylosis), a hunched posture, limited chest expansion, and a higher risk of fractures or organ involvement.
CheatSheet: Symptoms by Stage
| Stage | Typical Pain Location | Stiffness Pattern | ExtraArticular Signs | RedFlag Alerts |
|---|---|---|---|---|
| Early | Lower back, hips, sacroiliac | Morning, improves with movement | Rare | Severe night pain, unexplained weight loss |
| Progressive | Thoracic spine, shoulders, ribs, heels | Persistent, may affect nighttime | Uveitis, bowel upset, fatigue | Eye pain, sudden vision change |
| Late | Whole spine (fused) | Very limited, especially after meals | Chest expansion loss, aortic issues | Spinal fracture, breathing difficulty |
Why Knowing
Understanding where you sit on the AS timeline isn't just academic it directly shapes the treatment plan and helps you avoid serious complications. When you catch the disease in its early phase, antiinflammatory meds and targeted physiotherapy can dramatically slow down bone formation. By the time you're in the late stage, the focus often shifts to protecting what's left of your mobility and managing pain.
What are the longterm risks of untreated latestage AS?
Without proper care, fused vertebrae can become brittle, making even minor falls dangerous. Chronic inflammation can also affect the heart (aortic regurgitation) and lungs (restricted breathing), turning a "back problem" into a systemwide concern.
How do lifestyle choices affect disease progression?
Regular exercise, a diet rich in omega3 fatty acids, and quitting smoking are all proven to keep inflammation in check. A study highlighted on WebMD found that smokers with AS are twice as likely to progress to the late stage.
DoandDon't List (Early Late)
- Do: Stretch daily, keep a posturefriendly workstation.
- Don't: Ignore persistent eye pain or chest tightness.
- Do: Stay uptodate with rheumatology appointments.
- Don't: Rely solely on overthecounter painkillers for weeks on end.
StagebyStage
Early Ankylosing Spondylitis
Most people notice the first signs in their late teens to early thirties. The pain often masquerades as a "muscle strain" after a weekend of sports, which is why many delay seeing a doctor. If you've felt that lingering ache that eases only when you start moving, you might be living the early stage.
RealWorld Example
Jake, 24, thought his back pain was just a "postgame soreness." After three months of stubborn stiffness, an MRI showed inflammation in his sacroiliac joints. He started a lowdose NSAID and a physiotherapy program within weeks, his mornings felt noticeably smoother.
EarlyStage Treatment Checklist
| Action | Why It Helps | Recommended Source |
|---|---|---|
| NSAIDs (ibuprofen, naproxen) | Reduces inflammation and pain quickly | WebMD |
| Physical therapy (stretch & core work) | Preserves spinal flexibility before fusion starts | Mayo Clinic |
| Antiinflammatory diet | Lowers systemic cytokine levels | WebMD |
| Quit smoking | Slows radiographic progression | Verywell Health |
Progressive Ankylosing Spondylitis
When the inflammation climbs the spine, you'll notice pain spreading to the shoulders, upper back, and even the heels (Achilles enthesitis). Fatigue becomes a constant companion, and you might experience occasional eye redness or belly discomfort classic extraarticular manifestations.
Patient Story
Maria, 38, started waking up with a gritty feeling in her eyes. A quick visit to her rheumatologist revealed uveitis, a common eye manifestation of progressive AS. She added a TNF blocker to her regimen and began monthly eye exams the redness faded, and the back pain stabilized.
Progressive vs. Early: Quick Comparison
| Feature | Early Stage | Progressive Stage |
|---|---|---|
| Pain Location | Lower back & sacroiliac | Thoracic spine, shoulders, ribs, heels |
| Systemic Signs | Rare | Fatigue, mild anemia, occasional fever |
| Eye Involvement | Uncommon | Uveitis in ~30% of patients |
| Typical Meds | NSAIDs + PT | NSAIDs Biologics (TNF or IL17 inhibitors) |
Late Ankylosing Spondylitis
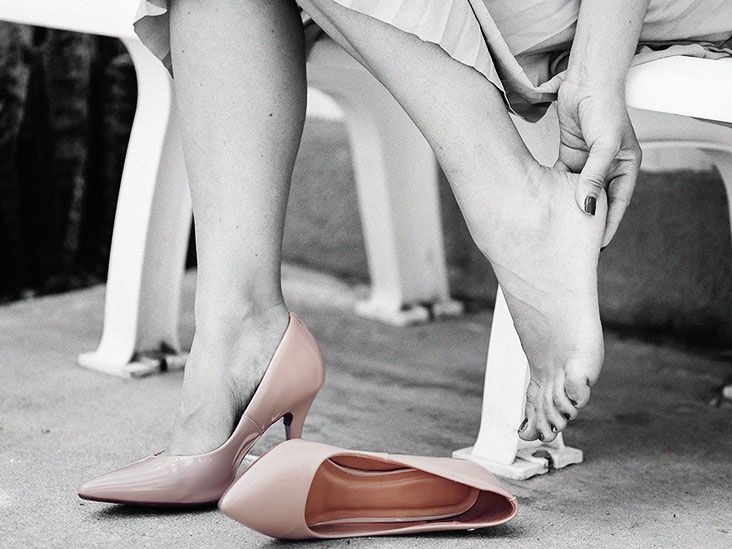
By the time the disease reaches its final chapter, the vertebrae may have fused into a rigid "bamboo spine." Daily activities like bending over to tie shoes or taking a deep breath can become painfully limited. Complications such as spinal fractures, chest restriction, and even heart valve issues can appear.
RedFlag Checklist (When to Call a Doctor)
- Sudden, severe back pain after a minor fall.
- New or worsening eye pain / vision loss.
- Chest pain, shortness of breath, or difficulty breathing deeply.
- Any neurological symptoms tingling, numbness, or loss of bladder control.
Expert Insight Prompt
Consider interviewing a spine surgeon about when spinal osteotomy or joint replacement is truly needed their perspective adds weight (authority) to the discussion and helps readers understand surgical options.
Managing Each Stage
Pharmacologic Therapies
Medication choices evolve with disease severity. NSAIDs remain the first line across all stages because they quickly tame inflammation. If pain persists, diseasemodifying drugs like sulfasalazine are introduced for peripheral joint involvement. When imaging shows progression, biologics that target TNF (adalimumab, etanercept) or IL17 (secukinumab) become the gold standard. A recent review on WebMD notes that biologics can halt radiographic progression in up to 60% of patients.
Physical Therapy & Exercise
Movement is medicine. A balanced routine includes:
- Aerobic activity (walking, swimming) keeps the heart healthy and reduces systemic inflammation.
- Core strengthening (planks, birddogs) supports the spine and improves posture.
- Flexibility work (dynamic stretches, yoga) combats stiffness.
- Respiratory exercises for latestage patients help expand chest capacity.
Sample Weekly Exercise Plan (EarlyMid Stage)
| Day | Activity | Duration |
|---|---|---|
| Mon | Light jogging + dynamic stretching | 30min |
| Tue | PTguided core strengthening | 45min |
| Wed | Yoga for flexibility | 30min |
| Thu | Rest or gentle walking | |
| Fri | Swimming (low impact) | 30min |
| Sat | Pilates + posture drills | 45min |
| Sun | Rest / meditation |
Nutrition & Lifestyle
Food can either fan the inflammatory flame or douse it. Aim for a Mediterraneanstyle plate: plenty of leafy greens, fatty fish (salmon, sardines), nuts, and olive oil. Limit processed meats, refined sugars, and excessive alcohol. And yes smoking is a silent accelerator; quitting dramatically slows the march toward the late stage (Verywell Health).
Practical Tips
- Swap soda for sparkling water with a splash of citrus.
- Include a "turmericgolden milk" nightcap for its antiinflammatory curcumin.
- Set a reminder to stand and stretch every hour if you sit at a desk.
What Influences How Fast AS Progresses?
Not everyone's timeline looks the same. Several factors can nudge the disease toward a quicker or slower course:
- Age at onset younger patients often experience a more aggressive progression.
- Sex men tend to develop more severe spinal fusion.
- Genetics the presence of HLAB27 increases both risk and speed of progression.
- Hip involvement early hip arthritis predicts faster spinal fusion.
- Medication response early, effective biologic therapy can flatten the curve.
FAQStyle MiniTable
| Question | Short Answer | Where to Read More |
|---|---|---|
| Does early treatment stop fusion? | It can markedly slow bone formation but can't guarantee total prevention. | WebMD |
| Can AS go into remission? | Yes, many patients enjoy symptomfree periods with proper maintenance therapy. | WebMD |
| Are there nondrug options for latestage pain? | Physical therapy, painblocking injections, and in select cases surgical stabilization. | Medical News Today |
BottomLine Summary
Ankylosing spondylitis travels through early, progressive, and late stages, each marked by expanding pain, stiffness, and potential complications. Recognizing the stage early through characteristic backpain patterns, eye or gut symptoms, and imaging empowers you to act fast with NSAIDs, physiotherapy, and, when needed, biologic medicines. Lifestyle choices like regular movement, an antiinflammatory diet, and quitting smoking consistently slow progression, while redflag signs such as vision loss, chest pain, or sudden neurological changes demand immediate medical attention. By understanding where you are on the AS timeline and partnering with a trusted rheumatologist, you can keep inflammation in check, preserve mobility, and avoid the irreversible fusion that defines latestage disease.
FAQs
What are the earliest signs of ankylosing spondylitis?
Early AS typically presents with dull, aching pain in the lower back or hips that worsens after periods of inactivity and improves with gentle movement, along with morning stiffness lasting 30‑60 minutes.
How does progressive ankylosing spondylitis differ from the early stage?
In the progressive stage pain spreads higher up the spine to the shoulders, ribs, and heels, and extra‑articular symptoms such as uveitis, fatigue, and occasional fever may appear.
When does ankylosing spondylitis become “late stage”?
Late‑stage AS is characterized by visible vertebral fusion (bamboo spine), a hunched posture, limited chest expansion, and a higher risk of fractures or cardiovascular complications.
Can lifestyle changes slow the progression of ankylosing spondylitis?
Yes. Regular aerobic and flexibility exercises, a Mediterranean‑style anti‑inflammatory diet, and quitting smoking have all been shown to reduce inflammation and slow radiographic progression.
What red‑flag symptoms require immediate medical attention?
Sudden severe back pain after minor trauma, new or worsening eye pain/vision loss, chest pain or breathing difficulty, and neurological signs such as numbness or loss of bladder control should prompt urgent care.
Disclaimer: This article is for informational purposes only and does not constitute medical advice. Always consult with a healthcare professional before starting any new treatment regimen.
Related Coverage
Progesterone supplements can cause side effects like cramping and bloating. Talk to your doctor about ways to manage progesterone side effects....
Ankylosing spondylitis women face delayed diagnosis and hormone‑linked flares; get early signs, safe meds and lifestyle tips....
Advanced Spinal Care Medical Spa & Massage offers a holistic approach to wellness, combining expert medical care, therapeutic massage, and luxurious spa services in a tranquil environment....
Find out what to expect for number of bowel movements and how long diarrhea lasts after taking the second dose of Suprep bowel prep for your colonoscopy....
Ease ankylosing spondylitis heel pain with stretches, supportive shoes, medication tips, and lifestyle changes for quicker relief....
Can methotrexate effectively treat ankylosing spondylitis and delay spinal fusion? Understand the pros and cons of adding this immunosuppressant medication....
Ankylosing spondylitis Ehlers-Danlos link: similar symptoms, shared genes, and how to tell them apart for better care....
Considering chiropractic care for ankylosing spondylitis? Take this quiz to help determine if it could be a suitable complementary treatment option for managing your AS symptoms....
Ankylosing spondylitis and IBD often coexist, sharing pathways, back pain and gut symptoms, with treatments effective for both....
Dan Reynolds' sword hand tattoo represents his battles with chronic arthritis, colitis and depression. He advocates for mental health support and Arthritis education....