Hey there, let's cut straight to the chase. ALS (amyotrophic lateral sclerosis) attacks the motor neurons that run through your spinal cord, and that's why you start noticing muscle weakness, twitches, and eventually difficulty breathing. Spotting these changes early can give you a head start on treatment, supportive care, and peace of mind.
In this guide you'll learn exactly how ALS harms the spinal cord, what early signals to watch for, how doctors confirm the diagnosis, and the best ways to live well with this motorneuron disease. Grab a cup of tea, settle in, and let's walk through it together.
ALS Impact on Spinal Cord
What part of the spinal cord is damaged in ALS?
The lateral corticospinal tracts and the anterior horn cells are the main victims. Those tracts carry signals from the brain to the muscles, while the anterior horn cells are the "finalstage" motor neurons that directly fire muscle fibers. When they degenerate, the signal chain breaks, leading to the hallmark weakness of ALS.
Why does damage start in the spinal cord before the brain?
ALS typically follows a "bottomup" pattern: lower motor neurons (in the spinal cord) show problems first, then upper motor neurons (in the brain) join the party. Think of it like a power outage that begins in the basement wiring before the main panel flickers. This progression is why early limb weakness is often the first clue.
What microscopic changes occur?
On a cellular level, proteins like TDP43 and SOD1 misfold and accumulate, glutamate builds up causing excitotoxicity, and oxidative stress damages the neuron's armor. These processes are welldocumented in research from Johns Hopkins Medicine, which underscores how the spinal cord's motor pathways bear the brunt.
How does spinalcord damage cause the classic ALS symptoms?
When those motor neurons die, muscles no longer receive the "moveme" signal. The result? Weakness, fasciculations (tiny muscle twitches), spasticity, and eventually trouble swallowing or breathing. It's a domino effectdamage in the cord translates directly into the ALS symptoms you might notice.
Is ALS considered a spinalcord disease?
Not exactly, but it's a motorneuron disease that heavily involves the spinal cord. Doctors often refer to it as ALS or "motor neuron disease" (MND). The term "spinal cord disease" can be misleading, because ALS also attacks brainstem and cortical neurons.
Recognizing Spinal Cord Damage
What early warning signs should I watch for?
- Unexplained weakness in one arm or leg, especially when you're climbing stairs or lifting a grocery bag.
- Persistent muscle twitches (fasciculations) that seem to pop up out of nowhere.
- Frequent tripping or dropping objects.
- Sudden fatigue that isn't fixed by rest.
These clues line up with the symptom checklist on Medical News Today.
How do symptoms differ if the upper vs. lower spinal cord is involved?
Uppermotorneuron signs include spasticity, exaggerated reflexes, and a "stiff" gait. Lowermotorneuron signs show up as muscle atrophy, weak reflexes, and those pesky twitching muscles.
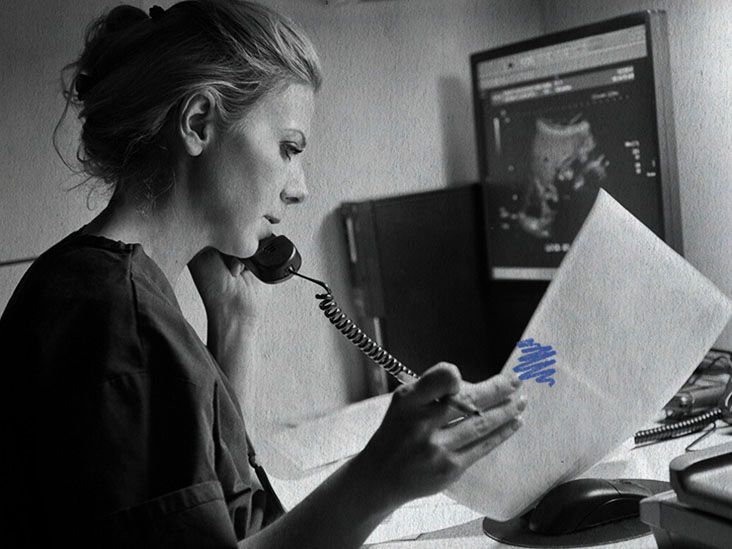
When should I call a doctor?
If you notice rapid progression (e.g., you can't lift a cup within weeks), trouble swallowing, or shortness of breath, pick up the phone now. Early referral can shave months off the diagnostic timeline and open doors to diseasemodifying therapies.
Can other spinalcord diseases mimic ALS?
Absolutely. Multiple sclerosis, cervical spondylotic myelopathy, and even a simple herniated disc can cause weakness and reflex changes. Below is a quick comparison:
| Condition | Typical Onset | Main Signs | Key Test |
|---|---|---|---|
| ALS | Adults 4070 | Mixed upper & lower motor signs, fasciculations | EMG + MRI (spine) |
| Multiple Sclerosis | 2040 | Sensory loss, optic neuritis, relapsingremitting | MRI brain & spine (lesions) |
| Cervical Spondylotic Myelopathy | 5070 | Neck pain, hand clumsiness, gait imbalance | MRI cervical spine |
| Herniated Disc | Varies | Localized radicular pain, weakness in specific myotome | MRI lumbar/spine |
What tests confirm spinalcord involvement?
Doctors usually start with an MRI of the whole spine to look for atrophy or lesions. Then, an electromyography (EMG) study shows denervation patterns that point to ALS. A lumbar puncture can rule out inflammatory causes, and blood tests check for genetic markers when familial ALS is suspected.
Diagnosing ALS Clearly
What imaging studies are most useful?
MRI is the gold standard. It visualizes cord thinning, hyperintensities, and helps exclude other pathologies. A CT scan isn't sensitive enough for early ALS changes.
How do electrophysiological studies work?
During an EMG, a tiny needle records electrical activity from muscles at rest and during contraction. In ALS, you'll see "fibrillation potentials" and reduced motorunit recruitment, confirming loss of motor neurons.
Are there biomarkers for spinalcord damage?
Neurofilament light chain (NfL) levels in blood or cerebrospinal fluid are rising as a promising marker of neuronal loss. Ongoing trials aim to make NfL a routine test for tracking disease progression.
What role does genetics play?
About 10% of ALS cases run in families, most often linked to mutations in the SOD1, C9orf72, or TDP43 genes. Genetic testing isn't mandatory for every patient, but it can guide family counseling and eligibility for certain clinical trials.
How long does the diagnostic process usually take?
From first symptom to confirmed diagnosis, many patients spend 612months navigating tests and specialist visits. The sooner you seek a neurologist experienced in motorneuron disease, the faster you'll get answers.
Managing Spinal Cord Damage
What medication can slow spinalcord degeneration?
Two FDAapproved drugs have modest effects: Riluzole reduces glutamatemediated excitotoxicity, and Edaravone scavenges free radicals. A newer combo, sodium phenylbutyrate/taurursodiol, targets protein misfolding and mitochondrial stress, showing early promise in clinical trials.
How do physical & occupational therapies help?
Therapists teach stretching routines that keep joints supple, strength exercises that preserve muscle mass, and adaptive strategies for daily living (e.g., using a rockerknife for dressing). One patient I spoke with said, "I'm still able to walk to the mailbox because my PT showed me a gentle treadmill program."
When is assistive technology needed?
As the disease advances, devices like powerassist wheelchairs, speechgenerating tablets, and noninvasive ventilation become gamechangers. Early planning means you won't be caught off guard when you need them.
What lifestyle changes support spinalcord health?
- Gentle aerobic activity (walking, swimming) to boost circulation.
- A balanced diet rich in omega3 fatty acids and antioxidants.
- Respiratory exercises (e.g., diaphragmatic breathing) to maintain lung capacity.
- Heat therapy or warm baths, which many ALS patients find soothing for stiff muscles.
These tips echo advice from leading ALS centers and help keep the body as strong as possible.
What support resources are reliable?
The ALS Association, local caregiver support groups, and reputable clinicaltrial registries (like clinicaltrials.gov) are trustworthy places to find information, emotional support, and research opportunities.
Future directions research targeting the spinal cord
Scientists are exploring genesilencing therapies (e.g., tofersen for SOD1linked ALS), antiTDP43 antibodies, and stemcell infusions aimed at protecting or even replacing damaged motor neurons. While many trials are still earlyphase, the momentum is encouraging.
Risks, Benefits & Myths
Is ALS contagious or caused by a spinal injury?
Nope. ALS isn't infectious, and while severe trauma may accelerate symptoms in a genetically predisposed person, it doesn't cause the disease.
Can diet or supplements cure spinalcord damage?
There's no solid evidence that any diet or supplement reverses ALS. Some antioxidants and omega3s may help overall health, but they're not a substitute for approved medications or comprehensive care.
Do all ALS patients eventually lose spinalcord function?
Progression varies. Some live 10+ years after diagnosis, especially with early multidisciplinary care. Others experience faster decline. Factors like age at onset, genetic type, and access to care influence the trajectory.
What are the biggest "gotchas" for patients?
Delayed diagnosis (often misattributed to arthritis or agerelated weakness), overlooking subtle breathing changes, and underutilizing assistive devices are common pitfalls. Staying proactive and asking the right questions can sidestep many of these.
Balancing hope and realism
It's okay to feel scared, but also remember that every new therapy, every supportive therapist, and every study participant pushes the boundary a little farther. Embrace hopeful possibilities while staying grounded in what the evidence says.
RealWorld Experiences
Case study: marathon runner turned ALS advocate
At 48, Alex noticed a strange twitch in his right hand that lingered after runs. Within six months, a neurologist confirmed ALS. Because he acted fast, he began a tailored physiotherapy regimen and kept training with a supportive coach. Today, he still runs short distances and uses a powerassist bike for longer outings.
Case study: teacher misdiagnosed with lumbar strain
Maria, 62, thought her leg weakness was a "bad back" from standing at the chalkboard. After months of worsening symptoms, a second opinion revealed ALS spinalcord involvement. The new diagnosis shifted her care toward speech therapy and homebased respiratory support, dramatically improving her quality of life.
Patient tip box
- Ask your neurologist for a copy of your EMG reportknowing the details helps you track progress.
- Keep a daily symptom diary; small changes become big clues for your care team.
- Don't underestimate the power of a good night's sleeprest supports nerve health.
- Connect with an ALS support group; shared stories can lift your spirit.
Conclusion
ALS spinal cord damage means the motorneuron highways that tell your muscles to move start to break down, leading to weakness, twitching, and eventually breathing challenges. By catching the early signsunexpected weakness, persistent fasciculations, or sudden fatigueyou can speed up diagnosis, start diseasemodifying meds, and bring in the right therapists and assistive tech.
Remember, you're not alone on this road. Reach out to a neurologist as soon as something feels off, join reputable support networks, and stay informed about emerging treatments that target the spinal cord headon. Together, we can navigate the uncertainties, celebrate the small victories, and keep hope alive.
FAQs
What are the first signs of ALS spinal cord damage?
Early indicators include unexplained weakness in a limb, persistent muscle twitches (fasciculations), frequent tripping, and sudden fatigue that doesn’t improve with rest.
How is ALS spinal cord damage diagnosed?
Diagnosis involves MRI of the spine to rule out other conditions, electromyography (EMG) showing denervation patterns, and sometimes blood or CSF tests for biomarkers like neurofilament light chain.
Can ALS spinal cord damage be treated?
While there is no cure, FDA‑approved medicines such as Riluzole, Edaravone, and the combo sodium phenylbutyrate/taurursodiol can slow progression, and multidisciplinary care improves quality of life.
When should I seek medical help for possible ALS spinal cord damage?
Contact a neurologist promptly if you notice rapid muscle weakness, difficulty swallowing, breathing changes, or if symptoms worsen within weeks.
What supportive technologies help people with ALS spinal cord damage?
Assistive devices like power‑assist wheelchairs, speech‑generating tablets, and non‑invasive ventilation, along with physical and occupational therapy, are essential for maintaining independence.
Disclaimer: This article is for informational purposes only and does not constitute medical advice. Always consult with a healthcare professional before starting any new treatment regimen.
Related Coverage
Master the right nasal spray technique to get effective relief from allergies and avoid common side effects....
Alpine ice core data uncovers ancient climate shifts, human impact, and environmental changes over 12 millennia in the European Alps....
Laryngeal cancer imaging guides you through CT, MRI, and PET scans, highlighting their uses, benefits, risks, and how they shape treatment plans....
Yupelri side effects often include dry mouth, cough and headache, while serious risks like urinary retention or eye pain need prompt care....
Find out the Zetia cost 2025, compare brand vs generic ezetimibe, and learn quick tips to lower your out‑of‑pocket price today....
Does Medicare cover Hoyer lifts? Yes, when medically necessary. Find out costs, requirements, and how to get one with Medicare....
Improve your daily comfort with posture and scoliosis management. Small changes can make a big difference....
Mpox outbreak is affecting Central and East Africa, especially children. Stay informed on symptoms, risks, and how to stay safe in 2025....
Medicare covers hyperbaric oxygen therapy for specific conditions like diabetic wounds and carbon monoxide poisoning. See if you qualify....
How IQ and decision-making connect in real life—beyond smarts, it's about patterns, patience, and avoiding overconfidence traps....