Understanding Your Risk of Melanoma Returning
When initially diagnosed with melanoma, many patients are fearful about the chances of their cancer coming back. Doctors use various tools to estimate the risk of the melanoma recurring after treatment of the primary tumor. By understanding what impacts your recurrence risk, you can take steps to lower the odds of melanoma returning.
Depth of Tumor Invasion
How deeply the melanoma has grown into layers of skin tissue is measured in millimeters (mm). The deeper the invasion, the higher the risk the cancer could spread. For example, 10-year recurrence rates range from 10-15% if less than 1 mm deep up to 55-70% if over 4 mm deep.
Presence of Ulceration
An ulcerated melanoma tumor has an open sore on the skin's surface leaking fluids. This speeds the spread of cancer cells and raises recurrence risk significantly. 10-year recurrence is approximately 30% without ulceration but can reach 75% if ulceration is present.
Number of Lymph Nodes Impacted
Lymph nodes act as filters for cancers spreading through the lymphatic system. The more nodes impacted, the wider the cancer has spread from the original site. Just having 1-3 lymph nodes involved indicates advanced disease with over a 70% chance of recurrence within 10 years.
Online Melanoma Recurrence Calculators
Doctors use statistical models based on clinical studies to estimate recurrence risks. Publicly available web calculators allow melanoma patients to plug in their parameters to assess odds without awaiting appointments.
Los Alamos National Laboratory Calculator
The Los Alamos RXcrisk calculator uses tumor thickness, ulceration, nodal status, age, and gender to provide 5 and 10-year recurrence rates. Graphs show how risk changes over time based on input factors.
Sunsmart Melanoma Calculator
Specific to Australian data, this calculator estimates recurrence rates out to 20 years post-treatment based on Breslow thickness, ulceration presence, and number of nodes involved. Comparison graphs display the impact of each variable on risk.
MedCalc Melanoma Survival Calculator
Using overall survival data from nearly 40,000 US melanoma patients, this tool calculates 1,3, and 5-year survival odds tailored to gender, age, stage, nodes examined, and number positive nodes. Includes comparisons to normal life expectancy.
Lifestyle Changes to Lower Recurrence Risk
While some risk factors for recurrence cannot be controlled, making certain lifestyle changes may significantly reduce your chances of melanoma coming back after successful treatment.
Practicing Sun Safety
Ultraviolet sun exposure is the main environmental cause of melanoma. Continuing good sun habits lowers the impact of damaging rays. Use sunscreen, wear protective clothing, avoid midday sun exposure, and examine skin regularly.
Nutritional and Dietary Approaches
Eating an antioxidant rich diet high in fruits, vegetables, and whole grains provides vitamins and minerals shown to inhibit cancer growth pathways. Additionally, maintaining a healthy body weight correlates with reduced recurrence risks across many cancers.
Stress Reduction Techniques
Chronic stress weakens the immune system over time. Relaxation practices such as meditation, yoga, massage, or counseling sessions help manage high stress levels. This can aid the body's natural defenses against development and spread of melanoma.
Avoiding Immunosuppresants
Medications or conditions hampering immune function allow cancers to grow unchecked. Patients should stop smoking and avoid alcohol abuse and unnecessary anti-rejection drugs. Treating illnesses like HIV or autoimmune disorders also helps.
Signs of Possible Melanoma Recurrence
Routine follow up skin exams, lymph node checks, and imaging tests help spot potential recurring melanoma. Contact your doctor promptly about any of the following:
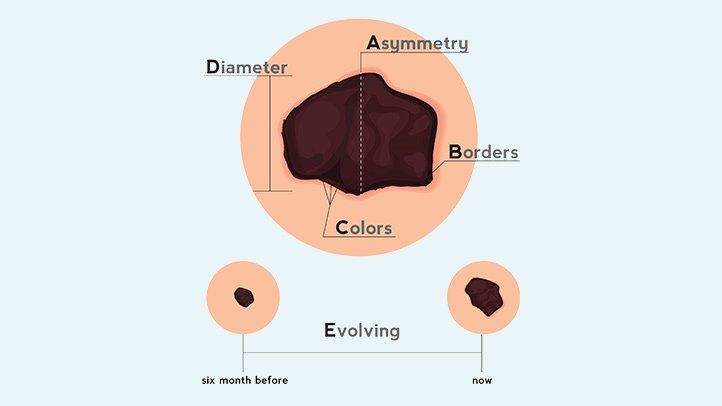
New Black or Dark Skin Growths
Appearance of asymmetric dark lesions with irregular borders signals possible melanoma returning. Use of dermoscopy and mole mapping highlights changes from previous skin exams.
Enlarged Lymph Nodes
Palpable lymph nodes near original melanoma could indicate cancer spread. Nodes sometimes emerge before new skin tumors if cancer has invaded the lymphatic system.
Ongoing Pain or Swelling
Unexplained pain, swelling, lumps, bone fractures, or neurological complaints prompt imaging tests checking for metastases in organs or bones. Catching spread early expands treatment options.
Elevated Blood Tumor Markers
Blood tests detecting elevated amounts of proteins like LDH indicate rapid cancer cell turnover in the body. Rising scores act as early warning system for disease progression.
Discussing recurrence risk estimates empowers patients to make informed health decisions. While daunting at first, taking positive steps to lower risk along with early detection of new tumors delivers hope for melanoma survivors.
FAQs
What are the most important factors affecting melanoma recurrence risk?
The depth of the original skin tumor, presence of ulceration, number of lymph nodes involved, and initial stage of diagnosis have the biggest impacts on recurrence odds.
How accurate are the online melanoma recurrence calculators?
The calculators provide estimates based on clinical study data of thousands of patients. Individual odds may vary, but they offer general guidelines regarding risk.
What lifestyle changes can reduce chances of melanoma returning?
Protecting your skin from sun exposure, eating a nutrient-rich diet, managing stress, avoiding immunosuppressants, and stopping unhealthy habits help lower recurrence risk.
What are signs to watch for that may indicate returning melanoma?
New asymmetric dark skin lesions, swollen lymph nodes near original site, unexplained pain or swelling, and rising blood tumor marker levels warrant promptly contacting your doctor.
Disclaimer: This article is for informational purposes only and does not constitute medical advice. Always consult with a healthcare professional before starting any new treatment regimen.
Related Coverage
Opening up to a therapist is critical for effective treatment but can feel challenging. Learn techniques to share intimate details and feel comfortable being vulnerable....
See pictures of what to expect during normal early stage mole removal healing vs. signs of complications. Get tips on minimizng scarring plus learn when atypical moles warrant urgent skin checks....
Discover the top morning teas to drink for health perks like weight loss, energy, and wellness. Includes tips for making green, black, herbal and other teas....
Get guidance on the top vitamins and supplements for women's health. Learn about key nutrients like folic acid, calcium, iron, vitamin D, omega-3s, and antioxidants....
Learn what to expect after 1 month on the slow carb diet. Average weight loss is 4-8 lbs from cutting refined carbs and increasing protein and fiber intake....
Melanoma signs, types, and pictures plus treatment options. Early detection and regular self‑checks can save lives....
Knowing the ABCDEs of melanoma is crucial for early detection. Learn the signs and symptoms, perform regular self-exams, and seek professional advice for suspicious moles....
Learn how to identify stage 1 melanoma moles using the ABCDE guidelines. See pictures, prognosis, treatment information for early stage melanoma caught before advanced spread....
Melanoma in situ, an early skin cancer, shows 98% five‑year survival; spotting and surgery or topical therapy give good results....
New research identifies genes that predict melanoma immunotherapy response, enabling personalized treatment plans for better outcomes....