Demystifying the Pronunciation and Meaning of Autoimmune Disease
When reading or hearing the term "autoimmune disease," you may find yourself tripped up on pronunciation or wondering about the meaning behind this category of complex conditions. By exploring proper pronunciation, analysis of the terminology, common examples, shared mechanisms, and more, we can grow appreciation for these diverse and often debilitating disorders.
Breaking Down the Term "Autoimmune Disease"
First, let's deconstruct the components of this medical name:
- "Auto" means self or one's own body.
- "Immune" refers to the body's built-in defense system against infection and illness.
- "Disease" describes a disorder disrupting normal health and function.
So in essence, "autoimmune disease" captures any condition characterized by one's own immune system mistakenly attacking healthy tissues and organs.
Phonetics of "Autoimmune Disease" Pronunciation
Since "autoimmune" is constructed from prefixes and suffixes added to the root word "immune," the pronunciation flows directly from these core parts:
- Auto: AW-toh
- Immune: ih-MYOON
- Disease: dih-ZEEZ
So properly vocalized, "autoimmune disease" should sound out as:
AW-toh-ih-MYOON dih-ZEEZ
What Defines an Autoimmune Disease?
Any condition fitting these criteria earns classification as an autoimmune disorder:
- An immune response targeting normal healthy cells due to failed self-recognition.
- Inflammation and tissue damage from this immune activity.
- Specific antibodies and white blood cells attacking the body's own proteins.
- Frequently, associations with certain genes and environmental triggers.
Additionally, autoimmunity tends to specifically damage tissue in contained areas or certain organ systems as opposed to widely across the whole body.
Common Examples of Autoimmune Diseases
Over 80 clinically defined autoimmune diseases exist affecting millions globally. Some of the most prevalent examples include:
Type 1 Diabetes
In type 1 diabetes, immune cells invade insulin-producing pancreatic islet cells. This lowers insulin leading to high blood sugar levels. Signs and symptoms include fatigue, excessive thirst, frequent urination, and weight loss.
Rheumatoid Arthritis
Here, inflammation stemming from autoimmunity attacks synovial joints. This brings swelling, stiffness, and damage over time. It commonly first affects smaller joints like those in the hands and feet.
Multiple Sclerosis
The immune system assaults the myelin sheath insulating nerve cells in the central nervous system. This disrupts messaging between the brain and body causing progressively worsening symptoms.
Inflammatory Bowel Diseases
Both Crohn's disease and ulcerative colitis feature immune activity inducing inflammation along parts of the digestive tract. Abdominal pain, severe diarrhea, fatigue and appetite loss frequently occur.
Psoriasis
Overactive immunity pathways result in skin cell overproduction and buildup. This manifests as plaques and scales, usually first appearing on the scalp, elbows, and knees.
Hashimoto’s Thyroiditis
The thyroid gland comes under assault. Inflammation and antibodies blocking thyroid hormones lead to problems like weight gain, mood changes, and feeling cold.
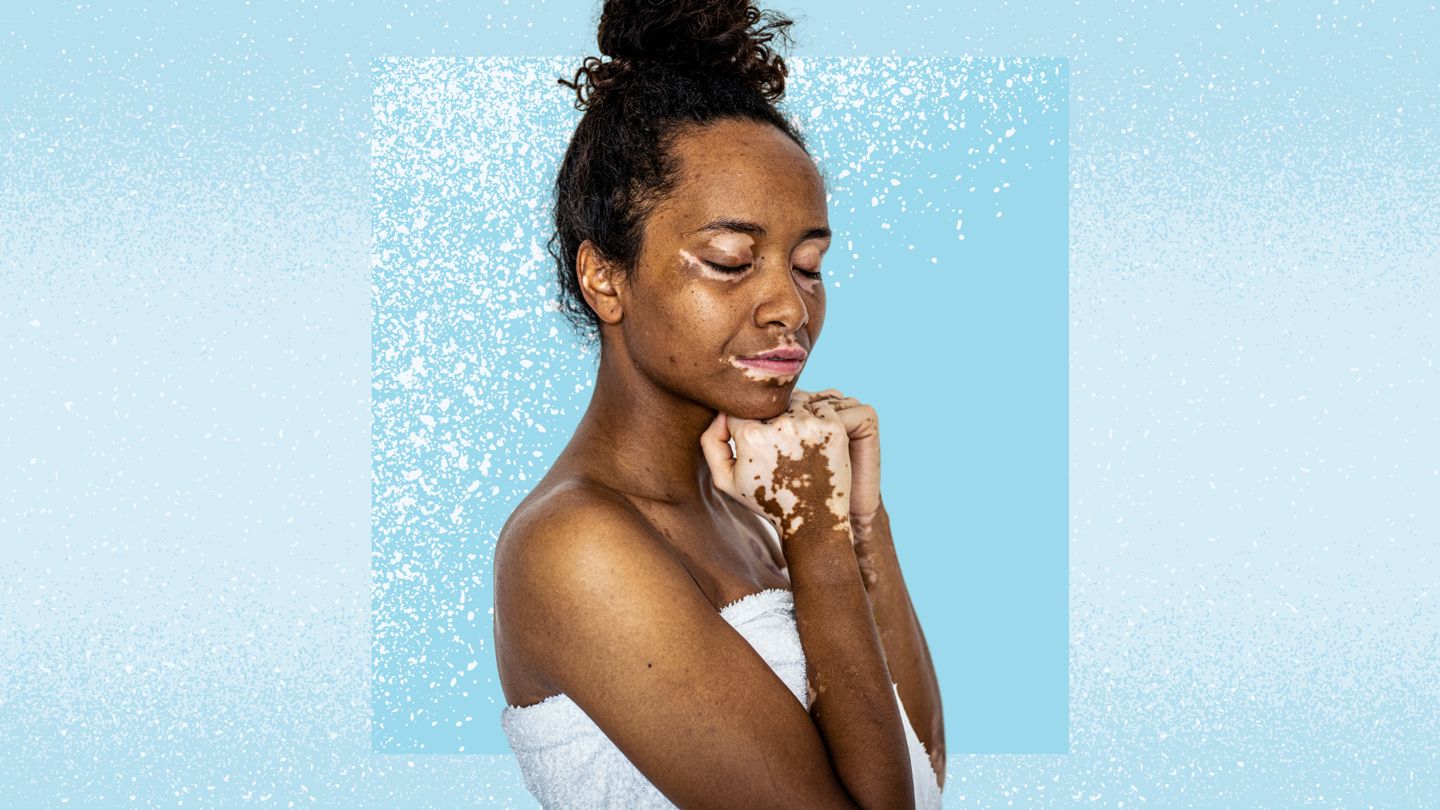
Vitiligo
This condition sees the immune system attack melanin-producing cells, leading to expanding white patches as skin pigmentation disappears. It typically first occurs on hands, feet, knees or face.
Shared Characteristics of Autoimmunity
While highly variable, autoimmune disorders often share underlying features and mechanisms that connect them as a broad disease classification. These include:
Inappropriate Immune Activation
The most unifying theme centers on immune cells and proteins mis-identifying healthy tissues as a threat and wrongly unleashing inflammation-provoking assaults upon them.
Central Role of Lymphocytes
Many autoimmune conditions feature either over-stimulated B cells generating auto-antibodies, T cells directed to attack self-structures, or dysregulation skewing lymphocytes towards self-reactivity.
Inflammation-Induced Damage
Chronic inflammation stemming from a wayward autoimmune response almost inevitably brings tissue destruction, scarring, cell death, organ dysfunction or remodeling.
Complex Causes
No single trigger determines someone's risk for developing an autoimmune disease. Interactions between genetic predispositions and environmental exposures together contribute towards risk.
Higher Incidence in Women
Across this disease category, women suffer disproportionate impact with some gender imbalances as high as 9:1 female to male ratios depending on the specific disorder.
Early Age Onset
While possible at any age, initial presentation often concentrates in childhood for some diseases and early-to-mid adulthood for others.
Theories Behind Autoimmune Disease Development
Researchers continue working to uncover why and how immune systems start attacking their own organs. No definitive mechanisms fully explain every autoimmune condition, but prevailing theories center around:
Molecular Mimicry
Foreign structures like viral or bacterial particles may resemble self-proteins enough to confuse immune cells and trigger unintended attacks hitting native cells.
Bystander Activation
Damage from an isolated immune reaction could spill over to inflame nearby healthy tissue and thereby expand autoimmune pathology.
Cryptic Antigens
Normally hidden internal cellular proteins when uncovered could look foreign enough to the body to initiate autoimmunity.
Loss of Regulatory T Cells
Declining numbers or functioning of cells that restrain overzealous immune responses allows harmful auto-reactivity to advance.
While hypotheses point to developmental pathways, ongoing research still seeks fuller illumination of mechanisms driving these disorders.
Diagnosing and Managing Autoimmune Diseases
Identifying and coping with autoimmune conditions poses challenges due to diffuse symptoms and dynamism over time. Key facets around establishing diagnoses and appropriate treatment include:
Specialized Testing
Lab tests checking for indicative autoantibodies and cell types allow for correctly differentiating autoimmune diseases from other possible conditions a patient might suffer from.
Monitoring Disease Activity
Tools like the erythrocyte sedimentation rate blood test, C-reactive protein, and imaging scans help gauge inflammation levels to guide medication adjustments responsive to flare-ups and remission cycles.
Managing Symptoms
Therapies aim to constrain immune over-activity and complications it incites. Corticosteroids, immunosuppressants, biologics, and newer treatments all intend to minimize autoimmune disease impact on health and quality of life.
While autoimmune conditions can't yet be cured or prevented outright, advancing medical capabilities continue expanding and improving long-term health prospects.
The Future Landscape of Autoimmune Disease
Great momentum drives autoimmunity research, bringing hope for transforming these diseases' trajectories. On the horizon, progress centers around:
Earlier Diagnosis
Detecting diseases at their onset or even predicting pre-clinical autoimmune vulnerability could enable faster intervention with better outcomes.
Personalized Medicine
Customizing therapies based on genetics, family histories, biomarkers and disease subtypes could make treatment more targeted and effective.
Emerging Treatments
Innovations like engineered T reg cells, antibody inhibitors, nanotechnology, intestinal microbiome modulation and more carry promise for selectively calming overactive immunity.
Prevention Strategy
While speculative, research around avoiding environmentally introduced triggers or promoting immunological tolerance may someday help curb autoimmune disease development.
As scientific capabilities advance, the pronunciations, meanings and manifestations of autoimmune diseases will hopefully become less ominous noises and more manageable conditions.
FAQs
How do you correctly pronounce "autoimmune disease"?
The proper pronunciation is: AW-toh-ih-MYOON dih-ZEEZ. It breaks down into the root words "auto," "immune," and "disease" from its Greek and Latin origins.
What qualifies a condition as an autoimmune disease?
Key criteria include: the body's immune system attacking its own healthy cells, inflammation and tissue damage from this process, antibodies/cells targeting the body's normal proteins, associations with certain genes and triggers, and localized injury to specific tissues or organs.
What are some examples of common autoimmune diseases?
Some of the most prevalent autoimmune diseases include type 1 diabetes, rheumatoid arthritis, multiple sclerosis, inflammatory bowel diseases like Crohn's and colitis, psoriasis, Hashimoto's thyroiditis, and vitiligo.
Who is most at risk for developing autoimmunity?
While possible at any age, women disproportionately suffer from autoimmune disorders over men. Family histories and certain gene variants also increase susceptibility. Peak initial onset centers in childhood for some diseases and young-to-middle adulthood for others.
Disclaimer: This article is for informational purposes only and does not constitute medical advice. Always consult with a healthcare professional before starting any new treatment regimen.
Related Coverage
Learn how to buy ruxolitinib Opzelura cream online to treat vitiligo patches. Understand treatment options, getting a prescription, using insurance, costs, and applying properly....
Segmental pigmentation disorder, also called vitiligo, is an autoimmune skin condition causing white patches from melanocyte destruction. Learn about vitiligo causes, diagnosis, treatments, prevention, and outlook....
Get clarity on properly pronouncing ...
Michael Jackson, Winnie Harlow, Jon Hamm, and other celebrities have opened up about their experiences with vitiligo. Learn how they're spreading awareness of this skin condition....
Opzelura is the first FDA-approved topical cream for restoring skin pigment in vitiligo patients. Learn about using Opzelura, expected results, side effects, and costs....
Tattoo ink fading and white spots happen, but can be prevented. Learn what causes tattoo fading, vitiligo spots, and the best methods to fix, cover, or embrace tattoo ink diffusion....
Learn the correct pronunciation for the fungal skin condition tinea versicolor. Breaking down the scientific name into tin-ee-uh ver-sih-cuh-lor prevents confusion and misdiagnosis....
Vitiligo affects Asians physically and emotionally at all ages. Learn about types, treatments and lifestyle adjustments to manage vitiligo from childhood through adulthood....
Dr. Elizabeth Yun is a top dermatologist providing customized treatments for chronic skin conditions like vitiligo, psoriasis, eczema, and acne. Learn about her services....
Terrence J, Michael Jackson, Winnie Harlow and other celebrities have spoken out about their experiences with vitiligo to reduce stigma and empower others with the condition....